DOL Temporarily Extends COBRA Sign-Up Deadlines
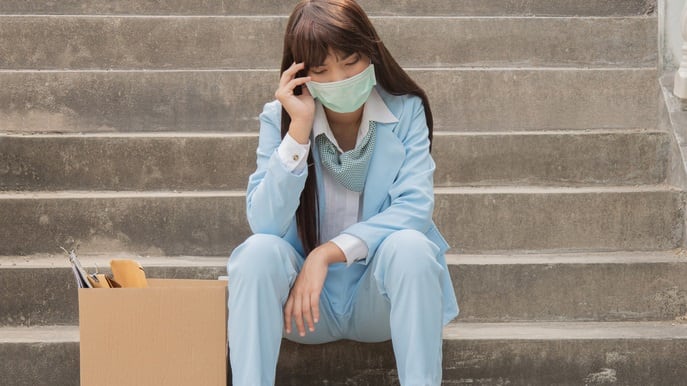
Terminated workers given more time to elect COBRA coverage and pay premiums
In response to the COVID-19 pandemic, the U.S. Department of Labor (DOL) and the IRS released a new final rule that temporarily extends the period in which eligible employees can elect COBRA health insurance coverage, and the deadline for them to begin making COBRA premium payments.
On May 4, the DOL and IRS jointly published Extension of Certain Timeframes for Employee Benefit Plans, Participants, and Beneficiaries Affected by the COVID-19 Outbreak. The final rule extends time frames affecting participants' rights to health care coverage, portability and continuation of group health plan coverage under COBRA, and it extends the time for plan participants to file benefit claims or appeal denied claims.
Along with the rule, the DOL posted a new set of COVID-19 FAQ’s for Participants and Beneficiaries.
"In light of the national emergency, the departments state that employers, employees and dependents may have difficulty meeting standard time frames," noted Brian Gilmore, lead benefits counsel and vice president at ABD Insurance & Financial Services in San Mateo, Calif. "The new final rule extends certain of those time frames to assist employers and employees in the process of maintaining employer-sponsored group health plan coverage."
Private sector employment decreased by 20,236,000 jobs from March to April, according to the April ADP National Employment Report. "Job losses of this scale are unprecedented," said Ahu Yildirmaz, co-head of the ADP Research Institute. "The total number of job losses for the month of April alone was more than double the total jobs lost during the Great Recession."
COBRA coverage can be a lifeline for employees who lost their jobs during the pandemic, allowing them to continue with a health plan they're familiar with, often at a cost lower than they could find through the Affordable Care Act marketplace.
New Rule's COBRA Provisions
The rule extends most COBRA deadlines to beyond the "Outbreak Period," which it defined as March 1, 2020, to 60 days after the end of the declared COVID-10 national emergency, or another date if provided by the agencies in future guidance. If the emergency declaration expires as written on June 29, 2020, the Outbreak Period will end on August 28, 2020, for instance.
No extension was granted for the 14-day deadline for plan administrators to furnish COBRA election notices.
- The COBRA election period. Under COBRA, employees and dependents who lose active coverage as a result of a qualifying event, such as termination of employment or reduction of hours, normally have 60 days to elect continuation of coverage after receiving a COBRA election notice. Under the rule, the 60-day timeframe doesn't start until the end of the Outbreak Period.
- The COBRA premium payment period. COBRA enrollees normally have 45 days from their COBRA election to make the first premium payment, and subsequent monthly payments must be made within a 30-day grace period that starts at the beginning of each coverage month. The new rule extends the initial premium payment and grace period deadlines beyond the Outbreak Period.
"An individual who experienced a qualifying event in April will have until 60 days after the end of the Outbreak Period within which to elect COBRA," explained Paul Yenerall, a Pittsburgh-based attorney with the law firm of Eckert Seamans Cherin & Mellott. "Similarly, any COBRA premiums due during the Outbreak Period will not be considered delinquent if the COBRA premiums are paid within 30 days following the end of the Outbreak Period. This means that COBRA premium payments that are due for March, April and May, at the very least at this point, are not required to be paid until 30 days after the end of the Outbreak Period."
Employers may require individuals to pay for COBRA continuation coverage. The premium that is charged cannot exceed the full cost of the coverage, plus a 2 percent administration charge. That cost is not affordable for many newly unemployed workers.
During the pandemic, however, some employers are choosing to pay for a former employee's COBRA coverage if the person has been laid off, or to do so for current employees who lost group health plan coverage when they were furloughed or had their hours reduced.
[SHRM members-only how-to guide: How to Administer COBRA]
Administrative Challenges
Employers and COBRA managers should prepare for the administrative challenges these deadline postponements will create for administering COBRA continuation coverage, Yenerall warned.
Similarly, attorneys at the law firm Winston & Strawn cautioned that "providing additional time for individuals to both elect and pay for COBRA coverage will create many complications for COBRA service providers, insurers, third-party administrators and group health plan sponsors and may leave providers and/or plans in the difficult position of having to provide and pay for services while an individual's status as a covered individual is uncertain."
Concerns were also expressed by Bobbi Kloss, director of human capital management services at Benefit Advisors Network (BAN), a Cleveland-based consortium of health and welfare benefit brokers. "The DOL attempted to clarify matters [relating to postponed COBRA and other benefit plan deadlines], with more confusing results and more undefined administration tasks for Human Resources professionals," Kloss said. "With the status quo continuously changing and an unknown as to when the national emergency ends, employers have one more 'to do' to add to their COVID-19 response plan."
Issues around adjusting COBRA notices also appear to be unresolved. "During the Outbreak Period, employers and plan administrators should consider supplementing and modifying…COBRA forms to reflect these extensions," noted attorneys at Sherman & Howard. Meanwhile, at the Groom Law Group, attorneys believe that "There is an open question whether employers need to revise COBRA notices to reflect the extended deadlines applicable to participants."
Related SHRM Articles:
Agencies Extend Various Employee Benefit Plan Deadlines, SHRM Online, May 2020
An organization run by AI is not a futuristic concept. Such technology is already a part of many workplaces and will continue to shape the labor market and HR. Here's how employers and employees can successfully manage generative AI and other AI-powered systems.



